Best Therapy for Depression:(Evidence Based) 2025 USA Depression affects over 21 million adults in the U.S. annually, making it one of the most prevalent mental health challenges. Fortunately, a range of therapies—backed by rigorous scientific research—offer hope and healing.
This article explores the most effective, evidence-supported treatments for depression, including emerging options like ketamine therapy and EMDR, and traditional approaches like CBT and talk therapy.
Introduction: Why Therapy Matters
Therapy is more than just talking—it’s a structured, evidence-based intervention that can rewire thought patterns, regulate emotions, and improve quality of life. Whether you’re dealing with major depressive disorder, treatment-resistant depression, or co-occurring anxiety, the right therapeutic approach can be life-changing.
1. Dialectical Behavior Therapy (DBT)
Overview:
DBT is a cognitive-behavioral therapy that blends mindfulness, emotion regulation, distress tolerance, and interpersonal effectiveness skills.
Key Components:
- Weekly individual therapy and group skills training.
- Emphasizes balancing acceptance and change.
- Originally developed for borderline personality disorder and suicidal behaviors.
Latest Research Insights:
- DBT shows significant improvements in depressive symptoms, especially in treatment-resistant depression.
- Adapted protocols (e.g., 16-session DBT skills training) outperform medication alone.
- Radically Open DBT (RO-DBT) targets overcontrolled personality traits often seen in chronic depression.
Strengths:
- Effective for emotional dysregulation and chronic depression.
- Reduces suicidal ideation and self-harm.
- Can be tailored for adolescents, veterans, and post-COVID patients.
Evidence:
A 2024 systematic review protocol published in PLOS ONE aims to evaluate DBT’s effectiveness for treatment-resistant depression. Early studies show significant symptom reduction when DBT is added to pharmacotherapy.
2. EMDR Therapy for Depression
Overview:
Originally developed for PTSD, EMDR uses bilateral stimulation (like eye movements) to help reprocess traumatic memories and reduce emotional distress.
Key Components:
- Eight-phase protocol including history-taking, desensitization, installation of positive beliefs, and body scan.
- Targets distressing memories that contribute to depression.
Latest Research Insights:
- EMDR significantly reduces depressive symptoms, especially in trauma-related or treatment-resistant cases.
- Meta-analyses show strong effect sizes (Hedges’ g = 0.75) for depression reduction.
- New protocols like DeprEND® focus specifically on depression-related cognitive patterns.
Strengths:
- Non-pharmacological and effective for patients with trauma histories.
- Can be delivered online or in group formats.
- Shows promise in reducing comorbid anxiety and improving emotional regulation
Evidence:
A 2024 meta-analysis found EMDR significantly reduces depressive symptoms, especially in severe cases. EMDR is endorsed by the World Health Organization and APA for trauma-related conditions.
3. Ketamine Therapy for Depression and Anxiety
Overview:
KAP combines the rapid antidepressant effects of ketamine with psychotherapy to enhance and prolong therapeutic outcomes.
Key Components:
- Ketamine is administered in low doses (IV or nasal spray).
- Therapy sessions are conducted during or after the ketamine experience.
- Focuses on emotional processing, insight, and integration.
Latest Research Insights:
- Ketamine shows rapid relief for treatment-resistant depression (TRD), often within hours.
- KAP may outperform ketamine alone in sustaining improvements and reducing comorbid symptoms like anxiety and PTSD.
- New ketamine metabolites (e.g., RR-HNK) show promise with fewer side effects.
Strengths:
- Effective for patients who haven’t responded to traditional antidepressants.
- Offers fast symptom relief, especially for suicidal ideation.
- Emerging evidence supports its use in combination with therapy for deeper healing.
Evidence:
A 2023 Harvard-led study found ketamine as effective as electroconvulsive therapy, with fewer side effects. A 2025 systematic review supports ketamine-assisted psychotherapy (KAP) for sustained symptom relief.
4. Interpersonal Therapy (IPT) for Depression
Overview:
IPT is a structured, time-limited therapy that focuses on improving interpersonal relationships and social functioning to reduce depressive symptoms.
Key Components:
- Targets four main problem areas: grief, role transitions, interpersonal disputes, and interpersonal deficits.
- Typically lasts 12–16 sessions.
- Emphasizes current relationships rather than past experiences.
Latest Research Insights:
- IPT is as effective as antidepressants in acute-phase treatment of depression.
- Particularly beneficial for individuals experiencing major life changes or relational stress.
- Long-term efficacy remains under-researched, but early studies suggest sustained benefits.
Strengths:
- Well-suited for people whose depression is linked to social or relational stress.
- Can be adapted for adolescents, postpartum depression, and even group formats.
Evidence:
A 2024 meta-analysis from Cambridge University Press found IPT comparable to antidepressants in efficacy. IPT is recommended by APA and WHO for mild to moderate depression.
Cognitive Behavioral Therapy (CBT) for Depression
In the United States, Cognitive Behavioral Therapy (CBT) plays a pivotal role in helping individuals manage and overcome depression. As a structured, short-term, and goal-oriented therapy, CBT empowers people to identify and challenge negative thought patterns that fuel depressive symptoms. It’s especially effective for those experiencing mild to moderate depression, and is often recommended as a first-line treatment by mental health professionals across the country.
You may also like: 15 Natural Ways to Treat Postpartum Depression (Evidence-Based)
CBT helps Americans with depression by:
Restructuring harmful thoughts:
Therapists guide patients to recognize distorted beliefs—like feelings of worthlessness or hopelessness—and replace them with more balanced, realistic perspectives.
Encouraging behavioral activation:
Individuals are supported in re-engaging with activities they once enjoyed, which helps counteract the withdrawal and inactivity common in depression.
Teaching coping strategies:
CBT equips people with practical tools to manage stress, solve problems, and navigate emotional challenges, fostering long-term resilience.
Expanding access through digital platforms:
Online CBT programs and teletherapy have made treatment more accessible, especially in rural or underserved areas.
Offering cost-effective care:
Studies show CBT is not only clinically effective but also economically viable, reducing long-term healthcare costs by preventing relapse and minimizing reliance on medication.
In a country where depression affects millions annually, CBT’s adaptability and evidence-based approach make it a cornerstone of mental health care.
Evidence:
CBT consistently ranks as one of the most effective therapies in randomized controlled trials and meta-analyses. It’s endorsed by the National Institute of Mental Health and APA.
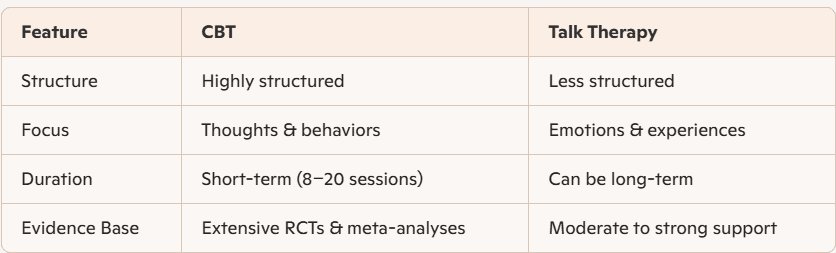
CBT Therapy vs. Other Modalities
While CBT is often used interchangeably with general talk therapy, it differs in its structured approach and emphasis on cognitive restructuring.
CBT vs. Talk Therapy:
Best Therapy for Depression: What the Research Says
There’s no one-size-fits-all answer. The “best” therapy depends on:
- Severity of symptoms
- Presence of trauma or anxiety
- Personal preferences
- Response to previous treatments
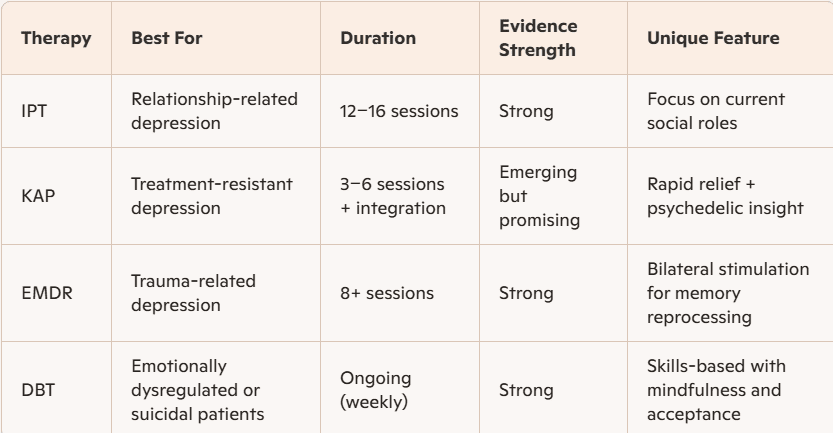
Top Evidence-Based Options:
- CBT: Best for structured, goal-oriented treatment
- EMDR: Ideal for trauma-related depression
- DBT: Effective for emotional dysregulation and suicidality
- Ketamine/KAP: Rapid relief for treatment-resistant cases
- IPT: Best for relational and situational depression
Talk Therapy for Depression: Still Relevant?
Yes! Talk therapy provides emotional support, insight, and coping strategies. While less structured than CBT, it remains a valuable tool, especially when combined with other modalities.
Conclusion: Choosing the Right Path
Depression is treatable, and therapy offers a personalized, evidence-based route to recovery. Whether you’re exploring CBT, EMDR, DBT, or ketamine-assisted psychotherapy, the key is finding a modality that aligns with your needs and goals.
References
- EMDR meta-analysis: MDPI Journal of Clinical Medicine, 2024
- DBT for TRD: PLOS ONE, 2024
Ketamine-assisted psychotherapy: Springer, 2025
- IPT vs. antidepressants: Cambridge University Press, 2024
- EMDR guidelines: EMDRIA
– [Choosing Therapy: CBT Techniques for Depression](https://www.choosingtherapy.com/cbt-for-depression/)
– [Psych Central: CBT for Depression](https://psychcentral.com/depression/cbt-for-depression)
– [Beck Institute: Treating Depression with CBT](https://cares.beckinstitute.org/how-cbt-can-help/depression/)
– [National Association of Cognitive-Behavioral Therapists](https://www.nacbt.org/)
– [Center for Deployment Psychology:
CBT-D](https://deploymentpsych.org/content/cognitive-behavioral-therapy-depression-cbt-d-0)